General Surgery-Categorical
Program Overview
 “Our mission is to train leaders in surgery and to train physicians who can operate in a community environment that holds to the highest ethical and professional standards and espouses the core surgical values of duty, honor and responsibility to patients.”
“Our mission is to train leaders in surgery and to train physicians who can operate in a community environment that holds to the highest ethical and professional standards and espouses the core surgical values of duty, honor and responsibility to patients.”
Welcome to the General Surgery Residency Program at the University of Washington Affiliated Hospitals! In the webpages to follow we hope to show you who we are in both the incredible depth and breadth of our program. The University of Washington provides extraordinary training in the robust intellectual environment of one of the top universities in the world. Like most university-based surgical programs, the University of Washington program provides a rigorous, comprehensive experience that is designed to produce the highest caliber surgeon. We are dedicated to the education of diverse individuals who will become future academic surgeon-leaders. In addition, we bear a special dual responsibility to train outstanding clinicians and community leaders for the suburban, rural, and even remote communities of the Northwest.
Our educational mission is to create exceptional surgeons who are clinically and technically superb while emphasizing continued learning, ethical principles, service, interpersonal relationships, and compassionate patient care. Our program is intellectually as well as physically challenging, with high expectations and standards for our trainees. One of the ways we distinguish ourselves from the handful of other elite programs is the incredible combination of a few things:
- The five states of Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI), comprising 27% of the U.S. land mass, serve as our geographic catchment area of tertiary and quaternary referrals for everything ranging from elective surgery to surgical complications and Level I trauma care. This provides an unmatched range of pathology.
- A top 10 U.S. Cancer Center which provides world-class surgical oncology.
- One of the leaders in trauma/critical care/burn care in the world in partnership with the renowned Life Flight Northwest.
- The six hospitals of UW Medicine, all university hospitals, each with a different care focus.
- A unique spirit of collegiality and collaboration which fosters a sense of camaraderie and community.
….All set in the extraordinary beauty of our environs of the Pacific NW – with green trees and flowers year around, and mountain peaks with water in every direction.
As the Program Director, my goal is to create an exciting, positive and progressive environment that fosters self-directed learning. With each new challenge we face in surgical education (e.g., 30% reduction in resident work hours in 2003) we want to IMPROVE the educational experience given new challenges, not just maintain the status quo. Finally, we want to do our part to redefine surgical training culture for the 21st century. One area of focus is working to change the 20th century view where residents train to finally become a surgeon at graduation—to a new philosophy of our entering junior surgeons training for five clinical years to become independent surgeons at graduation. The Pacific NW is the perfect setting for this in terms of shared goals of a community where everyone is pulling in the same direction and our flatter cultural hierarchies.
Thank you for your interest in our program! We all look forward to meeting you.
Rebecca P. Petersen, MD, MSc
Associate Professor of Surgery
Program Director, General and Preliminary Surgery
Quick Facts
Our residents:
- 50% are female
- 30% are URiM
Our program:
- Has been training surgeons since 1947
- Offers experience in robotic surgery (even as an R1).
- Provides a hybrid training model: typical university resident team structure and apprenticeship model training both used on different rotations.
- All of the faculty are full-time teaching faculty in the University of Washington School of Medicine, committed to surgical education. The majority are national and international leaders.
Our department community:
- Our Wellness Committee includes an equal number of faculty, residents and staff
- Our Diversity Council also includes faculty, residents and staff
- We focus on the development of the whole surgeon, emphasizing intellect, surgical skill, and humanity.
Program Leadership
Program Director, General and Preliminary Surgery
Practice: General Surgery, Complex Hernias and Abdominal Wall Reconstruction Surgery
Program Directors
Director, Resident Education in Quality & Patient Safety
Practice: Bariatrics, MIS General Surgery

Director, Technical Skills Education
Practice: Foregut, Complex Hernia Surgery, MIS
Associate Program Directors

Associate Program Director: Harborview Medical Center
Practice: Trauma/Critical Care Surgery

Associate Program Director, UW Medical Center-Northwest
Practice: General Surgery, Complex Hernia Surgery

Associate Program Director, UW Medical Center-Montlake
Practice: Bariatric Surgery, General Surgery, Metabolic, and Diabetic Surgery

Associate Program Director: VA-Puget Sound Health Care System
Practice: General Surgery, Critical Care Surgery
Associate Program Director: Harborview Medical Center
Practice: Trauma/Critical Care Surgery

Associate Program Director: Seattle Children’s Hospital
Practice: Pediatric Surgery
Clinical Experience
The comprehensive clinical training at the University of Washington can be matched at a handful of programs, but not exceeded! The ‘UW surgical product’ is well known and highly regarded around the country. Our graduates are routinely leaders in the top fellowship programs. For those who directly enter independent surgical practice, they seamlessly transition to their new community without further training.
We provide a rigorous experience with graduated responsibilities designed to produce the highest caliber surgeon. Our environment is intellectually challenging with high expectations and standards for all trainees. We span excellence in all aspects of surgical care from multi-disciplinary clinical evaluation, in-patient care, operative technique and decision making, management of post-op complications and team leadership.
The ingredients that comprise this elite training include:
- WWAMI region (Washington, Wyoming, Alaska, Montana and Idaho) catchment area for tertiary referrals. Our residents manage the most complex surgical patients available anywhere on a routine basis, so the straightforward patients become easy.
- World class Level I trauma/critical care and burn experience.
- Multi-disciplinary surgical oncology experience at the Fred Hutch Cancer Center, one of the top 10 cancer centers in the U.S.
- Pediatric surgery experience at Seattle Children’s Hospital, a quaternary referral center.
- High acuity surgery which includes learning from some of the top faculty in the country in: foregut surgery, colorectal, emergency general surgery, surgical oncology, endocrine, breast, bariatrics, thoracic, transplant, complex hernia and abdominal wall reconstruction.
- Minimally invasive and robotic surgery presence at all hospitals.
- A university level VA hospital.
- Large volume, bread and butter general surgery experience in an apprenticeship, community practice model.
Some statistics:
- Over 1000 major cases done as surgeon
- Over 350 cases completed by the end of the R2 year (far exceeding the 250 requirement)
- 3x required complex Stomach cases
- 4-5x required complex Esophagus, Liver, and Pancreas cases
- Facility with management of complex trauma/critical care
Training Sites
Six major hospitals and the clinics of the Fred Hutch Cancer Center are integrated into the general surgery teaching program: UW Medical Center-Montlake, UW Medical Center–Northwest, Harborview Medical Center, Puget Sound Veterans Administration Medical Center, Seattle Children’s Hospital, and Valley Medical Center. All hospitals are ~20 minutes apart around the Seattle urban area. Each hospital’s surgical service is staffed by full-time, world-renowned faculty members of the University of Washington School of Medicine. In our program, 100% of faculty at all hospitals are teaching faculty. Residents work closely with faculty in and out of the OR. Medical students rotate at each training site, giving our residents plenty of teaching opportunities.
 UW Medical Center-Montlake
UW Medical Center-Montlake
As the No. 1 hospital in Seattle and Washington State (U.S. News & World Report), UW Medical Center-Montlake is one of the world's foremost tertiary referral academic health centers, delivering exceptional, multidisciplinary care to patients who come to us from across the globe. Residents rotate at all levels at Montlake onto the following services: CT, Colorectal, Emergency General Surgery, Foregut, Hernia, Plastic, SICU, Surgical Oncology (Breast, Endocrine, HPB, Melanoma, Sarcoma) and Transplant Surgery. Services are typical university hospital team-based, academic services. Explore UW Medical Center-Montlake
 UW Medical Center-Northwest
UW Medical Center-Northwest
One hospital, 2 campuses; UW Medical Center-Northwest is a community-based center about 20 minutes north of Montlake. Our residents rotate here during the R2 and R3 years where they do high volume, bread and butter general surgery cases in a 1:1 apprenticeship model. The UW Medicine Hernia Center is based at the Northwest campus where it attracts both routine hernia patients and those requiring complex abdominal wall reconstruction. Explore UW Medical Center-Northwest
 Fred Hutch Cancer Center
Fred Hutch Cancer Center
The Fred Hutch Cancer Center is listed as one of the top 10 cancer centers in the U.S. (U.S. News and World Report). It is the No. 1 cancer hospital in the Pacific Northwest and Washington state's only National Cancer Institute (NCI)-designated comprehensive cancer center. Fred Hutch Cancer Center research provides world-class cutting-edge approaches to cancer treatment and prevention. Their goal is to lead the world in translating scientific discovery into the prevention, treatment, and cure of cancer. Our residents participate in multi-disciplinary cancer clinics and Tumor Boards at the Fred Hutch Cancer Center at all levels of residency. Explore Fred Hutch Cancer Center
 Harborview Medical Center
Harborview Medical Center
As the only designated Level I adult and pediatric trauma and regional burn center in the state of Washington, Harborview Medical Center serves as the regional trauma and burn referral center for Alaska, Montana and Idaho and the disaster preparedness and disaster control hospital for Seattle and King County. This 413-bed world-class teaching and research hospital is owned by the county and managed by the University of Washington. It is the home of Airlift Northwest. Harborview provides specialized care for a broad spectrum of patients from throughout the Pacific Northwest, including the most vulnerable residents of King County. Residents at all levels rotate at Harborview Medical Center onto typical university hospital surgical teams and work side by side with some of the most renowned traumatologists in the world. Rotations include: Burn, ED, Plastic Surgery, Thoracic, Trauma, Trauma SICU, and Vascular. Explore Harborview Medical Center
 Seattle Children’s Hospital
Seattle Children’s Hospital
Seattle Children’s is the only regional pediatric referral center devoted to the needs of children ages birth to 21 in the four-state area of Washington, Alaska, Montana and Idaho – the largest referral region of any children’s hospital in the country. Resident rotations at Seattle Children’s occur in the R1 and R3 years. Residents work closely with faculty on a typical university hospital team at the main campus. The R3 runs a sub-service giving them leadership opportunities. During the week, a resident may travel to the Seattle Children’s Bellevue or Everett surgical clinics working 1:1 with an attending for a full day of routine pediatric surgery cases. Explore Seattle Children’s Hospital
 VA Puget Sound Health Care System
VA Puget Sound Health Care System
Since 1923, VA Puget Sound Health Care System has distinguished itself as a leader in teaching, research and patient care while earning prestigious recognition in serving the health care needs of more than 112,000 Veterans living in 14 counties around the Puget Sound in the Pacific Northwest. With a reputation for excellence, innovation and extraordinary care of our Nation’s heroes, the VA Puget Sound Health Care System is a university level VA and a regional referral site for VA's northwest region, VA Puget Sound Health Care System provides care for Veteran populations encompassing Alaska, Montana, Idaho and Oregon. Our VA receives the second highest level of funding in the US. Residents rotate at the VA during their R1, R3 and R5 years on the General Surgery team. As R4s, the residents take a chief role on the Vascular Surgery team. Explore VA Puget Sound Health Care System
 Valley Medical Center
Valley Medical Center
Founded as a public district hospital in 1947, Valley Medical Center is a 321-bed, acute care community hospital of UW Medicine that serves more than 600,000 residents in Southeast King County. Residents rotate here at the R4 level for a high volume, bread and butter general surgery experience in an apprenticeship model. Explore Valley Medical Center
Rotations
The University of Washington program provides a rigorous and comprehensive experience with graduated responsibilities designed to produce the highest caliber surgeon. It is intellectually challenging with high expectations and standards for all trainees. Our comprehensive curriculum encompasses both didactics provided through a wealth of teaching conferences and focused technical instruction provided through open, laparoscopic and robotic technical laboratories. We developed the innovative EVATS rotation for our surgical residents and published this in 2003. The EVATS rotation provides time for Emergency coverage, Vacation time, Academic time, and Technical Skills training.
First Year
Day one of the R1 year starts your journey from junior surgeon to independent surgeon. Focus areas include initial patient evaluation in the clinic, ICU and emergency room and operative and perioperative care across a wide variety of disciplines. Rotations include acute care surgery, trauma, surgical oncology, burns, colorectal, vascular, thoracic, and pediatric surgery. These services are rounded out with experiences in emergency room trauma, critical care, burn surgery, and plastic surgery. On all services, the R1 assists in operations on his/her patients and performs appropriate operative procedures. Our R1’s perform approximately 150 cases and procedures.

Second Year
The R2 concentrates on the fundamentals of critical care, with primary responsibility in the University of Washington CTICU and the Harborview Trauma ICU. Rotations on other services, such as transplant surgery, surgical oncology, acute care surgery, and vascular surgery and the general surgery service at Northwest Hospital broaden this experience. The R2 performs operative procedures that build on the skills learned in the first year. By the end of the R2 year our residents have performed over 350 cases, far exceeding the 250 minimum requirement.
Third Year
The R3 year commences the senior resident years. Residents spend the year solidifying general surgery experiences at the VA and UW Medical Center, where advanced laparoscopy and bariatric surgery is the focus. At Harborview, the R3 functions as the primary trauma surgery consultant and leads the trauma ward service in conjunction with a Chief resident. A rotation as a senior fellow in medical gastroenterology augments the R3’s knowledge and expertise in upper and lower GI endoscopy. The R3 also serves as the chief resident on the burn surgery, pediatric surgery and Northwest Hospital community general surgery rotations. These chief-level rotations introduce the R3 to administrative and team leadership roles.
 Fourth Year
Fourth Year
With the operative experience, leadership skills and surgical maturity gained during the R3 year, the R4 focuses on a more complex surgical experience. Rotations include hepatobiliary surgery, surgical oncology, endocrine, colorectal surgery and advanced laparoscopic surgery at UW and vascular surgery at the VA. On the Harborview trauma services the R4’s serve in the Chief role. A highpoint of the year is the Valley Hospital rotation where the R4 works 1:1 in an apprenticeship type role with attendings in this busy community hospital.
 Chief Year
Chief Year
The Chief resident year is the year where you assemble all the elements of your training and demonstrate to the faculty that you’re ready to become an independent surgeon. With the graduated responsibility and appropriate supervision provided from your first day in the program as a junior surgeon, our Chief residents exercise major responsibility in patient care, leadership, teaching, and administrative areas. Chief residents perform the most complex operative procedures and assume responsibility for the operative and supportive care of all surgical patients at each of our major teaching hospitals. As leaders in the program, they also participate extensively in the education of medical students and residents, clinical investigations, and in departmental and service administrative matters. Rotations include trauma, general surgery, acute care surgery, colorectal and surgical oncology. Flexible training options are available in the Chief year.
Conferences

The UW Department of Surgery focuses on the development of the total surgeon in the three areas of intellect, skills and humanity. In addition to the usual bedside, clinic, and operating room teaching activities, more formal teaching conferences occur on two levels: department-wide and hospital-based.
Department-Wide
Grand Rounds
Department of Surgery Grand Rounds is held once per month at the University hospital. Speakers include national and international leaders in surgery as well as some of our own UW faculty. Residents have the opportunity to engage all visiting professors in roundtable discussions specifically designed for resident education.
Hospital-Based
Each of our teaching hospitals has a weekly QI Conference (aka ‘M&M’). We strongly believe that review of surgical outcomes and problem-based learning and improvement should be an ongoing pursuit that is woven into the fabric of a surgeon’s daily practice. For this reason, we incorporate review of NSQIP and Washington State SCOAP data into our weekly QI conferences. We also have a large selection of conferences at each hospital based on the clinical emphasis of its services. Some examples are listed below:
UW Medical Center-Montlake
- QA/QI Conference (aka ‘M&M’)
- Team Building and Mentorship Conference – Wednesday. The Program Director meets with each class monthly on a rotating basis (each week a different class). Variety of topics discussed. (Lunch provided)
- How-I- Do-It (HIDI) Conference – Thursday AM. Faculty present their approach to unique surgical problems along with clinical pearls. (Breakfast provided)
- Surgery Team Midday Care Conference (SToMaCh) – Tuesday. Joint conference for faculty and residents. Variety of topics discussed. (Lunch provided)
- Chairman’s Conference – Thursday afternoon. Focused on topic selected by Chairman and Chief resident. Informal setting, generally focused on leadership, ethics and an informal curriculum.
- Transplant
- CT
UW Medical Center-Northwest
- QA/QI Conference (aka ‘M&M’
- Multidisciplinary Breast Conference- A review of pathology, imaging and oncologic options for upcoming cases
Harborview Medical Center
- QA/QI Conference (aka ‘M&M’)
- Trauma Conference – Monday. Presentations by faculty, fellows, residents on a variety of topics. (Lunch provided)
- Vascular Surgery Morning Conference – Tuesday. (Breakfast provided)
- Trauma ICU Didactics – Tuesday AMs. Unofficially termed ‘Maier Rounds’ for Dr. Maier, overnight admissions presented to the Trauma service.
- Trauma Journal Club – Monthly. (Lunch provided)
- Chest Conference – Thursday. Case presentations in ICU and Pulmonary medicine. (Lunch provided)
VA Hospital
- QA/QI Conference (aka ‘M&M’)
- GI Radiology conference
- Surgery – Pathology conference
- Angiography conference (Vascular Surgery service)
Seattle Children’s Hospital
- QA/QI Conference (aka ‘M&M’)
- Weekly didactic teaching conference
- Pathology conference
Fred Hutch Cancer Center
- Multidisciplinary Cancer Conferences – specific to Breast, Colorectal, Endocrine, Foregut, Liver, Lung, Pancreatic, and Sarcoma services. (Lunch provided)
Program-Led
Surgical Science Series
Wednesday morning is a time to enjoy the company of fellow residents and faculty from around the system, to catch up on the latest advances and help foster the camaraderie, fellowship and community that make residency a positive experience. Our weekly didactic conference occurs in a 4 hour, bi-monthly block of time on Wednesday mornings known as the Surgical Science Series. The junior resident sessions occur twice a month and focus on building a foundation in basic general surgical principles. The senior resident sessions occur twice a month on alternate Wednesdays and focus on classical reviews of the surgical literature and evidence-based approaches to specific topics. Some highlights:
- Curriculum: American Board of Surgery’s SCORE curriculum
- Held at a central location. (Breakfast provided)
- Zoom option is available (and recorded for later viewing)
- The flipped classroom format is used. The topic is assigned in advance with an interactive, discussion-based format headed by a faculty member expert in that area.
- Each 4-hour session is divided
- 2-hour didactic portion (roundtable discussion and mock-oral board questions)
- 2-hour second session for technical skills/simulation or our expanded curriculum in leadership, quality, coding & billing, academic mentoring, palliative care, residents as teachers, professionalism, global surgery, surgical ethics, and practice management-related topics.
Journal Club
Our residents moved our monthly Journal Club from a restaurant to a faculty home in order to further develop our community. (Dinner provided)
ABSITE Prep
Our Director of ABSITE and Board Review hosts a monthly ABSITE Prep Conference in the fall months preceding the ABSITE.
Simulation Training
 |
 |
 |
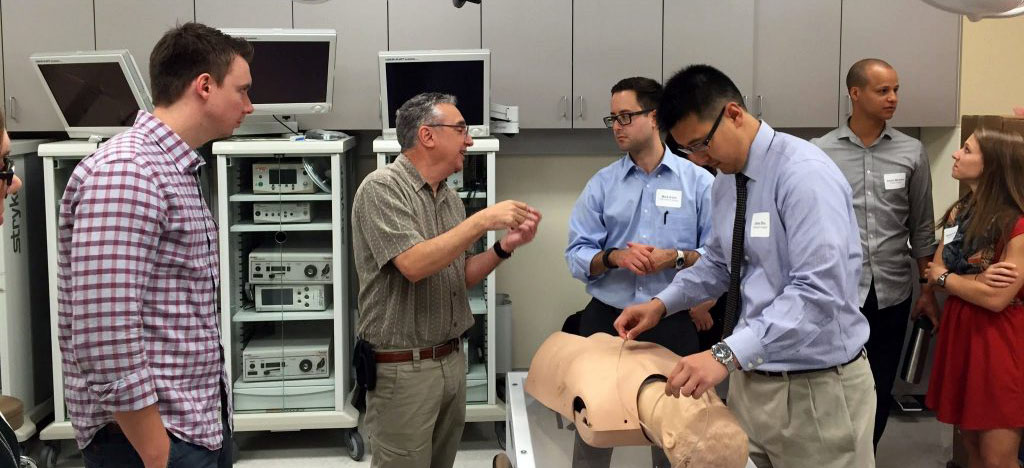 |
The WWAMI Institute for Simulation in Healthcare (WISH) is University of Washington’s state-of-the-art simulation center for health education. Our center was one of the first Level 1 ACS accredited simulation labs in the United States. WISH was spearheaded by leaders in the Department of Surgery in 2007, and under the influence of our multidisciplinary faculty has expanded to include a 2000 sq. ft. facility at UW Medical Center and an 8000 sq. ft. facility at Harborview Medical Center. WISH is a unique resource for our residents that embodies the Department of Surgery’s commitment to innovation in medical education.
Our residents have 24/7 access to surgical equipment, suture material, laparoscopic trainers, and virtual reality modules. This ease-of-access has led our surgical residents to heavily utilize the simulation facilities for independent practice. Every year of training, surgical residents have protected time during their EVATS rotation to advance their technical skills as part of a structured curriculum at each training level that includes modules in robotic and laparoscopic surgery, ultrasound imaging, endoscopy, central line and chest tube placement, surgical airway procedures and advanced trauma life support. These modules eventually lead to certification in Robotics, Fundamentals of Laparoscopic Surgery (FLS), and Fundamentals of Endoscopy Surgery (FES). Very popular with our residents, is our annual Laparoscopic Rodeo and Robotic Olympics competitions, with prizes for the top performers.